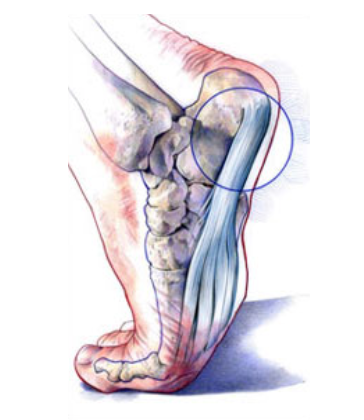
Plantar fasciitis is inflammation of the ligament under the heel. Heel spurs occur in muscle deep to the plantar fascia and were originally thought to be the cause of the pain. We now know that they form in response to local inflammation, with the body forming bone mistakenly in its attempt to repair the plantar fascia and do not contribute at all to the pain.
In general, plantar fasciitis is a self-limiting condition. Unfortunately, the time until resolution is often six to 18 months, which can lead to frustration for patients and physicians. Rest was cited by 25 percent of patients with plantar fasciitis in one study as the treatment that worked best. Athletes, active adults and persons whose occupations require lots of walking may not be compliant if instructed to stop all activity. Many sports medicine physicians have found that outlining a plan of “relative rest” that substitutes alternative forms of activity for activities that aggravate the symptoms will increase the chance of compliance with the treatment plan.
It is equally important to correct the problems that place individuals at risk for plantar fasciitis, such as increased amount of weight-bearing activity, increased intensity of activity, hard walking/running surfaces and worn shoes. Early recognition and treatment usually lead to a shorter course of treatment as well as increased probability of success with conservative treatment measures.
STRETCHING AND STRENGTHENING
Stretching and strengthening programs play an important role in the treatment of plantar fasciitis and can correct functional risk factors such as tightness of the gastrocsoleus complex and weakness of the intrinsic foot muscles. Increasing flexibility of the calf muscles is particularly important. Frequently used stretching techniques include wall stretches and curb or stair stretches
Strengthening programs should focus on intrinsic muscles of the foot. Exercises used include towel curls and toe taps. Exercises such as picking up marbles and coins with the toes are also useful. To do a towel curl, the patient sits with the foot flat on the end of a towel placed on a smooth surface. Keeping the heel on the floor, the towel is pulled toward the body by curling the towel with the toes. To do toe taps, all the toes are lifted off the floor and, keeping the heel on the floor and the outside four toes in the air, the big toe is tapped to the floor repetitively. Next, the process is reversed, and the outside four toes are repetitively tapped to the floor while keeping the big toe in the air.
SHOES
A change to properly fitting, appropriate shoes may be useful in some patients. Some individuals wear shoes that are too small, which can exacerbate many types of foot pain. Patients often find that wearing shoes with thicker, well-cushioned midsoles, usually made of a material like high-density ethylene vinyl acetate (such as is found in many running shoes), decreases the pain associated with long periods of walking or standing.
ARCH SUPPORTS AND ORTHOTICS
Patients with low arches theoretically have a decreased ability to absorb the forces generated by the impact of foot strike. The three most commonly used mechanical corrections are arch taping, over-the-counter arch supports and custom orthotics. Arch taping and orthotics were found to be significantly better than use of NSAIDs, cortisone injection or heel cups in one randomized treatment study.
CORTICOSTEROID INJECTIONS
Corticosteroid injections, are usually reserved for recalcitrant cases. A plain radiograph of the foot or calcaneus may be obtained before injecting steroids to ensure that the cause of pain is not a tumor. Steroids can be injected via plantar or medial approaches with or without ultrasound guidance. Potential risks include rupture of the plantar fascia and fat pad atrophy.
SURGERY
In cases that do not respond to any conservative treatment, surgical release of the plantar fascia may be considered. Plantar fasciotomy may be performed using open, endoscopic or radiofrequency lesioning techniques.